FEMALE INCONTINENCE SURGERY

FEMALE INCONTINENCE SURGERY
Surgery and procedures for stress incontinence
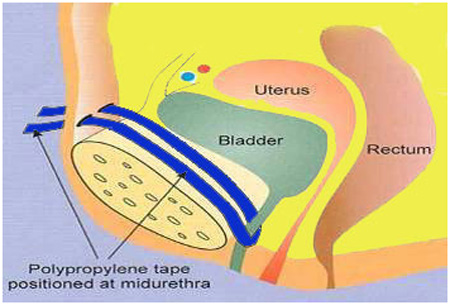
Tape procedures
Tape procedures can be used for women with stress incontinence. A piece of plastic tape is inserted through a cut (incision) inside the vagina and threaded behind the tube that carries urine out of the body (urethra).
The middle part of the tape supports the urethra, and the two ends are threaded through two incisions in either the:
- tops of the inner thigh - this is called a transobturator tape procedure (TOT)
- tummy (abdomen) - this is called a retropubic tape procedure or tension-free vaginal tape procedure (TVT)
By holding the urethra up in the correct position, the piece of tape can help reduce the leaking of urine associated with stress incontinence.
The effectiveness of these tape procedures is similar, with around two in every three women not experiencing any leaking afterwards.
Even those who still have some leaking after surgery often find this is less severe than it was before the operation.
However, it is not uncommon for women to need to go to the toilet more frequently and urgently after this procedure, and some find they are unable to completely empty their bladder when they go to the toilet.
In some cases, the tape can wear away or move over time and further surgery may be needed at a later stage to adjust it – for example, to make it looser - or remove it.
Colposuspension
Colposuspension involves making an incision in your lower abdomen, lifting up the neck of your bladder, and stitching it in this lifted position.
This can help prevent involuntary leaks in women with stress incontinence.
There are two types of colposuspension:
- open colposuspension – where surgery is carried out through a large incision
- laparoscopic (keyhole) colposuspension – where surgery is carried out through one or more small incisions using special small surgical instruments
Both types of colposuspension offer effective long-term treatment for stress incontinence, although laparoscopic colposuspension needs to be carried out by an experienced laparoscopic surgeon.
Problems that can occur after colposuspension include difficulty emptying the bladder fully when going to the toilet, recurrent urinary tract infections (UTIs), and discomfort during sex.
Sling procedures
Sling procedures involve making an incision in your lower abdomen and vagina so a sling can be placed around the neck of the bladder to support it and prevent accidental urine leaks.
The sling can be made of:
- a synthetic material
- tissue taken from another part of your body (autologous sling)
- tissue donated from another person (allograft sling)
- tissue taken from an animal (xenograft sling), such as cow or pig tissue
In many cases, an autologous sling is used and will be made using part of the layer of tissue that covers the abdominal muscles (rectus fascia). These slings are generally preferred because more is known about their long-term safety and effectiveness.
The most commonly reported problem associated with the use of slings is difficulty emptying the bladder fully when going to the toilet.
A small number of women who have the procedure also find they develop urge incontinence afterwards.
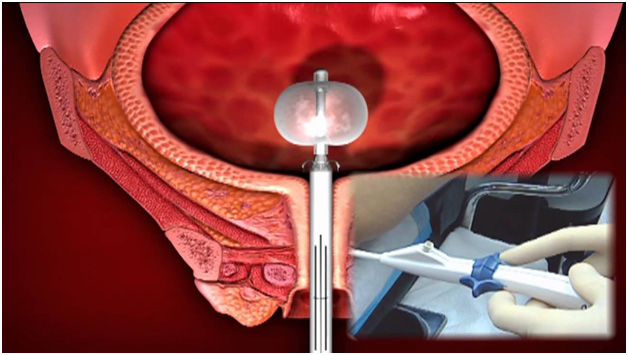
Urethral bulking agents
A urethral bulking agent is a substance that can be injected into the walls of the urethra in women with stress incontinence. This increases the size of the urethral walls and allows the urethra to stay closed with more force.
A number of different bulking agents are available, and there is no evidence one is more beneficial than another.
This is less invasive than other surgical treatments for stress incontinence in women as it does not usually require any incisions.
Instead, the substances are normally injected through a cystoscope inserted directly into the urethra.
However, this procedure is generally less effective than the other options available. The effectiveness of the bulking agents will also reduce with time and you may need repeated injections.
Many women experience a slight burning sensation or bleeding when they pass urine for a short period after the bulking agents are injected.
Artificial urinary sphincter
The urinary sphincter is a ring of muscle that stays closed to prevent urine flowing from the bladder into your urethra.
In some cases, it may be suggested that you have an artificial urinary sphincter fitted to relieve your incontinence.
This tends to be used more often as a treatment for men with stress incontinence and is only rarely used in women.
An artificial sphincter consists of three parts:
- a circular cuff that is placed around the urethra – this can be filled with fluid when necessary to compress the urethra and prevent urine passing through it
- a small pump placed in the scrotum (when used in men) that contains the mechanism for controlling the flow of fluid to and from the cuff
- a small fluid-filled reservoir in the abdomen – the fluid passes between this reservoir and the cuff as the device is activated and deactivated
The procedure to fit an artificial urinary sphincter often causes short-term bleeding and a burning sensation when you pass urine.
In the long-term, it is not uncommon for the device to eventually stop working, in which case further surgery may be needed to remove it.
Surgery and procedures for urge incontinence
Botulinum toxin A injections
Botulinum toxin A (Botox) can be injected into the sides of your bladder to treat urge incontinence and overactive bladder syndrome.
This medication can sometimes help relieve these problems by relaxing your bladder. This effect can last for several months and the injections can be repeated if they help.
Although the symptoms of incontinence may improve after the injections, you may find it difficult to fully empty your bladder.
If this happens, you will need to be taught how to insert a thin, flexible tube called a catheter into your urethra to drain the urine from your bladder.
Botulinum toxin A is not currently licensed to treat urge incontinence or overactive bladder syndrome, so you should be made aware of any risks before deciding to have the treatment. The long-term effects of this treatment are not yet known.
Sacral nerve stimulation
The sacral nerves are located at the bottom of your back. They carry signals from your brain to some of the muscles used when you go to the toilet, such as the detrusor muscle that surrounds the bladder.
If your urge incontinence is the result of your detrusor muscles contracting too often, sacral nerve stimulation – also known as sacral neuromodulation – may be recommended.
During this operation, a device is inserted near one of your sacral nerves, usually in one of your buttocks. An electrical current is sent from this device into the sacral nerve.
This should improve the way signals are sent between your brain and your detrusor muscles, and so reduce your urges to urinate.
Sacral nerve stimulation can be painful and uncomfortable, but some people report a substantial improvement in their symptoms or the end of their incontinence completely.